Understanding the Causes of Retinal Detachment
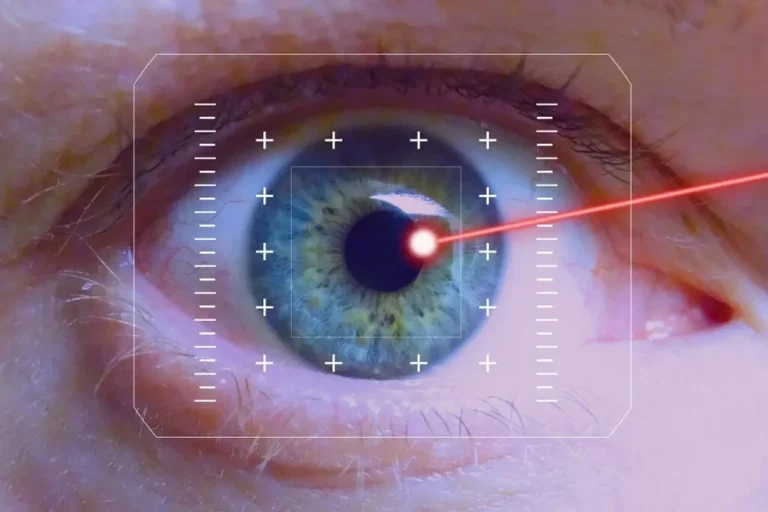
The retina is a thin layer of light-sensitive tissue at the back of the eye. It converts light into signals that travel to the brain via the optic nerve, enabling vision. The retina must remain attached to the underlying blood vessels to receive oxygen and nutrients. If retinal detachment occurs, visual processing is disrupted, and vision is threatened.
What Is Retinal Detachment?
Retinal detachment occurs when the retina separates from its normal position at the back of the eye. This condition is painless but presents with specific symptoms. Common symptoms include a sudden increase in floaters and flashes of light in the affected eye, as a rapid onset or large number of these may indicate that the retina has detached. A key sign of detachment is a dark shadow or curtain moving across the visual field; this shadow usually starts in peripheral vision and may spread toward the center.
What Causes It?
Retinal detachment has three main forms, each with different underlying causes. Rhegmatogenous retinal detachment is the most common type. It occurs when a tear or hole forms in the retina, allowing vitreous fluid from the center of the eye to pass through and collect beneath the retina. This fluid separates the retina from the underlying tissue.
The tractional form of detachment occurs when scar tissue develops on the retina’s surface, which can pull the retina away from the back of the eye as the tissue contracts. It is commonly linked to systemic conditions that damage retinal blood vessels, particularly diabetic retinopathy. This is a condition where prolonged high blood sugar leads to vessel damage and scar formation. In the exudative type of detachment, fluid collects under the retina without a tear or hole. The resulting pressure separates the retina from the choroid.
How Is It Treated?
Treatment aims to reattach the retina and seal any breaks or holes, and the procedure used depends on the type and severity of detachment. During a pneumatic retinopexy, a surgeon injects a gas bubble into the vitreous cavity. The bubble presses the retina against the eye wall at the site of the tear. Laser surgery is then performed to close the tear.
Scleral buckling places silicone around the eye to compress it inward, which aims to bring the wall closer to the detached retina and promote reattachment. The surgeon can also drain the fluid that accumulated under the retina. For cases with significant traction or severe tears, vitrectomy involves removing the vitreous gel that is pulling on the retina. The surgeon replaces the vitreous to keep the retina in position during healing.
Speak With an Eye Surgeon
The degree of vision recovery after retinal detachment surgery depends on how much of the retina was detached and whether the macula was affected. Care after surgery can include specific head positioning and other best practices. If you experience symptoms such as sudden flashes of light, an increase in floaters, or a shadow in your vision, seek prompt evaluation by an eye surgeon for diagnosis and treatment options.